Chapter 5: How To Enter Value-Based Payment Arrangements

This post is part of a series of blog posts aimed at unpacking value based payment for primary care practices looking to make the transition to value based care. Click here to read more about how Elation supports the transition to value based payment.
By: Dr. Sara Pastoor & Jessica Sullivan
We've spent the last few chapters explaining the characteristics of different value-based payment (VBP) arrangements and where they fall along the HCP-LAN continuum.
But how do practices enter into these VBP arrangements? In short, clinicians can participate in value-based payment models by contracting with a payer group (i.e., Aetna) or applying to participate in a program for Medicare or Medicaid (i.e., Primary Care First). There are two main tracks to contracting with payers: contracting as an individual practice or joining a larger group of practices.
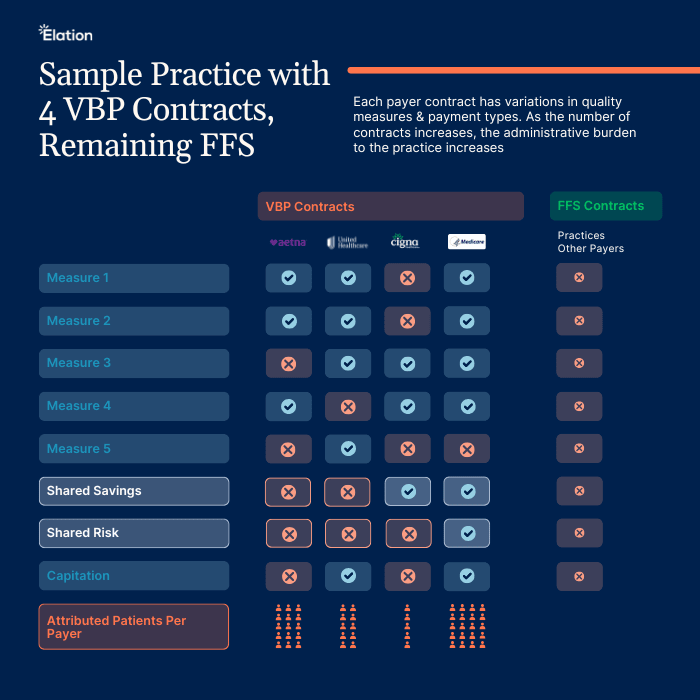
These features are crucial to understand because when a payer designs a VBP contract, they negotiate (or even unilaterally decide) the terms of the contract and there can be a lot of variability in contracts. In fact, multiple VBP contracts per practice may look very different from each other. This is part of what makes entering into VBP so complicated! In other words, what results is a unique blend of requirements that the participating practice would need to follow - with more difficult requirements imposed for contracts in higher HCP-LAN categories.
Participating through a program
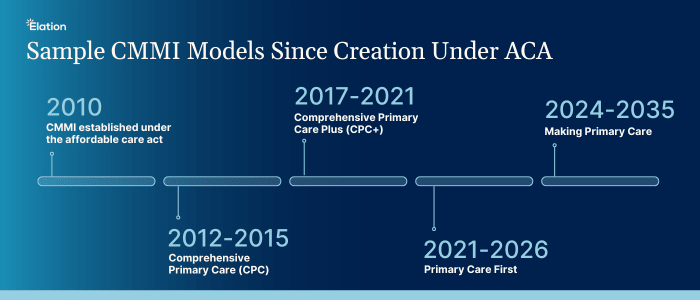
The most common way for individual practices to pursue a value-based payment contract is through an established program. Unsurprisingly, CMS has been at the forefront of creating many of these programs and some commercial payers also offer contracts of their own. In 2010, CMS established the Center for Medicare and Medicaid Innovation (CMMI) - also known as the CMS ‘Innovation Center.’ CMMI was established as a result of the Affordable Care Act to design, test, and study new value-based payment models.
Since its inception, CMMI has launched over 60 programs. Because these programs are managed by CMS, they only affect reimbursements for Medicare and/or Medicaid beneficiaries. Many of the programs are also specifically built for PCPs since primary care plays such an impactful role in a value-based paradigm.
CMMI programs often intentionally offer different participation tracks that span across the different HCP-LAN categories. This spectrum of options lowers the barrier to entry for those who have never participated in value-based payment contracts before. Practices can apply for the program track that best aligns with their interest, level of experience, and ability to take on risk.
Commercial payers
Commercial payers are private insurance companies - for example, Blue Cross Blue Shield, Aetna, Cigna, etc.
Commercial payers are increasingly offering alternative payment models (APMs) to reimburse clinicians through VBP as opposed to fee-for-service.
An example of a standardized type of VBP contract is called a Medicare Advantage (MA) contract. Medicare Advantage is healthcare coverage that a person aged 65 and older can purchase directly from a commercial payer rather than from CMS. Medicare Advantage offers expanded benefits compared to traditional Medicare (e.g. dental and vision coverage), so it can be seen as a more attractive alternative for seniors, although network restrictions, plan complexity, and unexpected out of pocket costs are common patient complaints, and the quality of plans varies widely.
Joining an organization
Since making the transition to VBP can be daunting administratively and financially, clinicians often team up with other clinicians to reduce the administrative and financial burden of VBP.
Physicians can form organizations or networks of clinicians. Clinicians affiliate so they can gain resources and expertise to further their VBP goals. Examples of these types of organizations can include:
-
Independent Physician Associations
-
Clinically Integrated Networks
-
Accountable Care Organizations
-
Medical Groups
Benefits of joining a larger organization:
-
Access to technology
-
Operational expertise & support
-
Economies of scale when purchasing technology/equipment and negotiating contracts
-
Maintaining independence while also increasing revenue through value-based payments
-
Pool of providers and patients lowers financial risk of unexpected, astronomical expenses
A bird’s eye view of VBP participation
In a nutshell, there are a multitude of ways today for practices to venture into VBP arrangements! The wide range of program and contract types allows them to select the ones that they feel the most prepared for and gives them the opportunity to move further down the HCP-LAN continuum as they gain experience and confidence. To learn how to navigate contract negotiation and choose the best arrangement to create success, read our Six Essential Tips for Value-Based Success.






