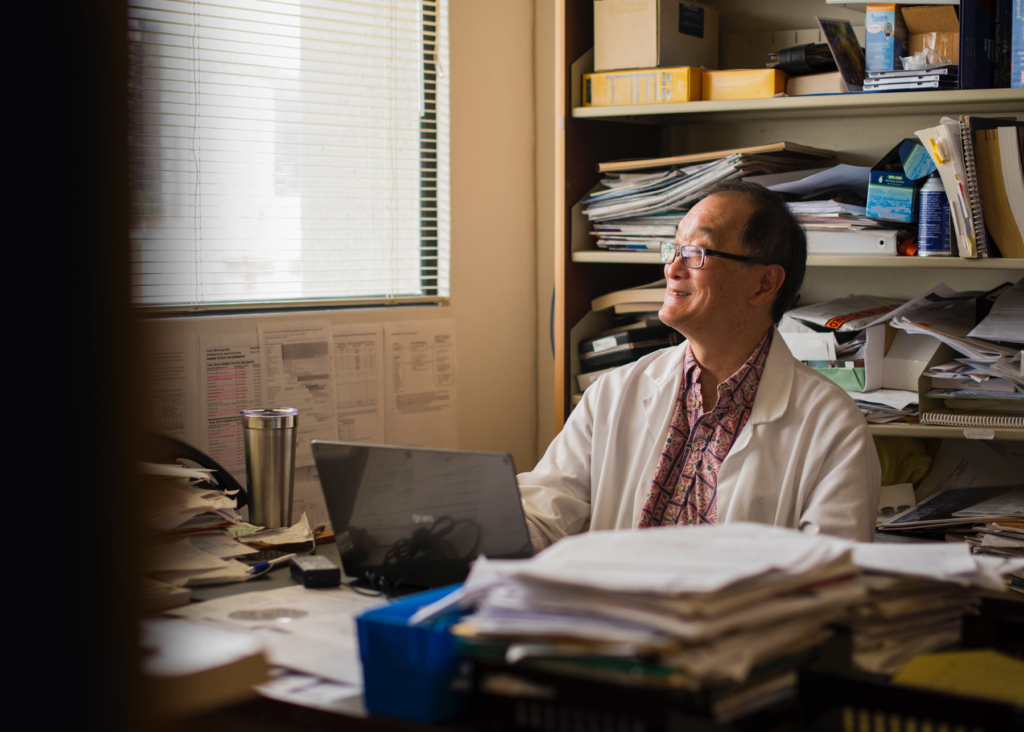
The patient always comes first: How a Hawaiian physician thrives in independent primary care
As a teenager in Hawai’i, Roger Kimura walked a path that seemed preordained.
Every good grade he earned in science and math, each encouraging comment from a teacher, and the types of jobs available to math whizzes reinforced this trajectory. He was destined to become an engineer. He knew it, and so did everyone else.
Then, during college, something changed. “Rather than working with numbers and blueprints and being stuck in an office somewhere,” Dr. Kimura says, “I found that I liked working with people who were more specifically trying to help people.” Suddenly, years of working toward an engineering career melted away to reveal another option: medicine.
Growing up, Dr. Kimura and his peers never considered becoming physicians. Medicine was for the elites, not them. But that assumption changed when he began volunteering at the Queen’s Medical Center in Honolulu, the state’s only Level 1 trauma center, which had been established more than a century earlier in part with donations from community members. Free of today’s regulations, he got in on the action by transporting patients, delivering lab specimens, and watching doctors save lives. “You could see the potential of medical care, where you could take broken people or sick people and bring them back to life,” he recalls. “It just seemed like something I could see myself doing.”
A patient’s physician
Now, 36 years into practicing medicine in Honolulu, Dr. Kimura can hardly imagine doing anything else.
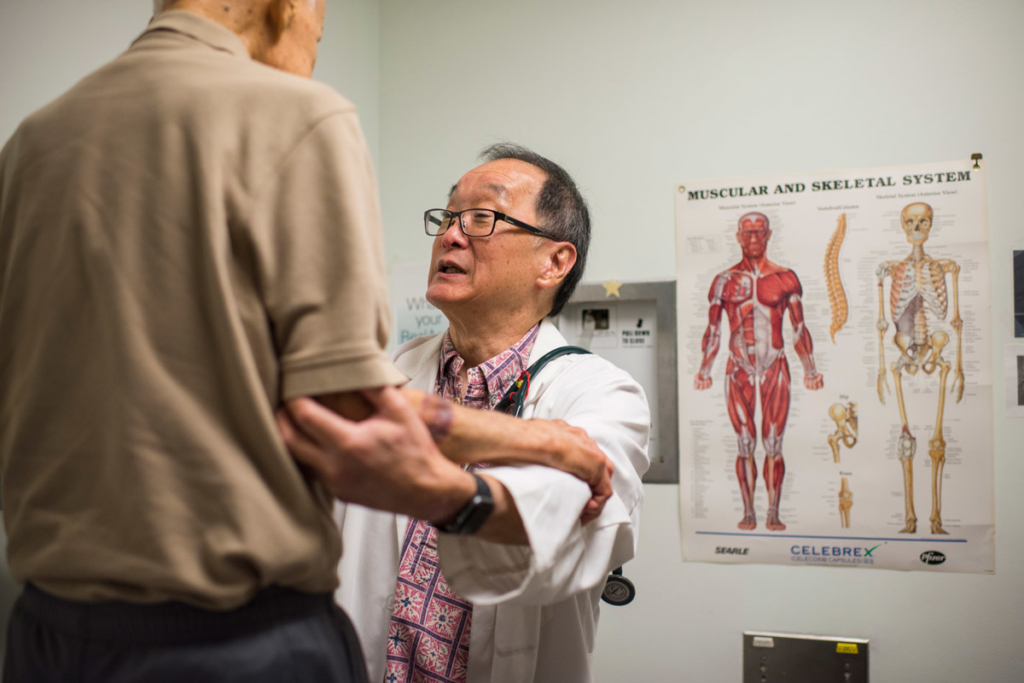
His independent primary care practice is geared more around patients than maximizing profits. Once, he briefly scrapped his Saturday morning hours, only to renege upon receiving disappointed phone calls. He accepts fewer patients than many doctors — and, consequently, less reimbursement — to ensure that he has roughly 30 minutes for each appointment. (Just 11 percent of physicians spend 25 or more minutes with each patient, according to a 2018 survey.) Dr. Kimura even makes the infrequent house calls for patients who have no other choice. Patients return the love by gifting souvenirs from their vacations or doing favors for Dr. Kimura and his staff of two.
If there’s one thing other than medicine that bonds his primary care practice and his patients, it’s a strong sense of community. This principle stems from Dr. Kimura’s childhood role as a young uncle, charged with playing leader and caregiver to his nieces and nephews. The result is a practice centered on his patients, his neighbors, his home. But it’s possible only because of his status as an independent primary care practitioner and the success he has achieved in a changing, consolidating market.
Ultimately, it’s about service,” Dr. Kimura notes. “The patient may not always be right, but the patient always comes first.”
Independent primary care and innovation
When one longtime patient became too ill to leave the house, Dr. Kimura made a home visit to treat the patient and meet with their domestic partner and caregiver. The patient eventually passed away. Not long after, Dr. Kimura took an appointment with the caregiver, who was concerned about her hypertension. But the physician noticed something else: She appeared to be suffering from hallucinations. If he hadn’t known her situation or scheduled enough appointment time, Dr. Kimura might’ve overlooked this second patient’s need for more serious treatment.
He referred the patient to a brand-new integrated behavioral health program, a recent partner of his practice. If Dr. Kimura was a physician in a larger, more mechanistic organization, he might have been so mired in the grind of seeing as many patients as possible that he would never have noticed the patient’s changing condition — or been able to recommend the best path for her treatment.
His independence has mandated that he stay aware of innovation and be nimble enough to embrace it. For instance, Dr. Kimura has participated in a new value-based payment initiative that provides monthly per-member incentive payments, the national advanced primary care medical home model called Comprehensive Primary Care Plus (CPC+). His own professional satisfaction, meanwhile, has encouraged him to help struggling colleagues. He joined a feedback group to improve Centers for Medicare and Medicaid Services programs. He became a Hawaiian delegate to the American Medical Association. And he has long advocated for solutions to physician burnout, at first by attempting to mentor younger colleagues and then by pushing for better burnout assessments, a numbers-driven task suited to a doctor who almost became an engineer.
“Part of my personal mission is to also serve the family of medicine, so that’s why I need to get involved in these other things,” Dr. Kimura shared. His commitment to his colleagues became yet another avenue through which he could find and build community.
Part of my personal mission is to also serve the family of medicine.”
Succeeding in independent primary care
While Dr. Kimura built a practice that is uniquely his, the tools and tips he offers can apply to physicians everywhere. Although success is no easy task in independent primary care, he suggests his is due to the following:
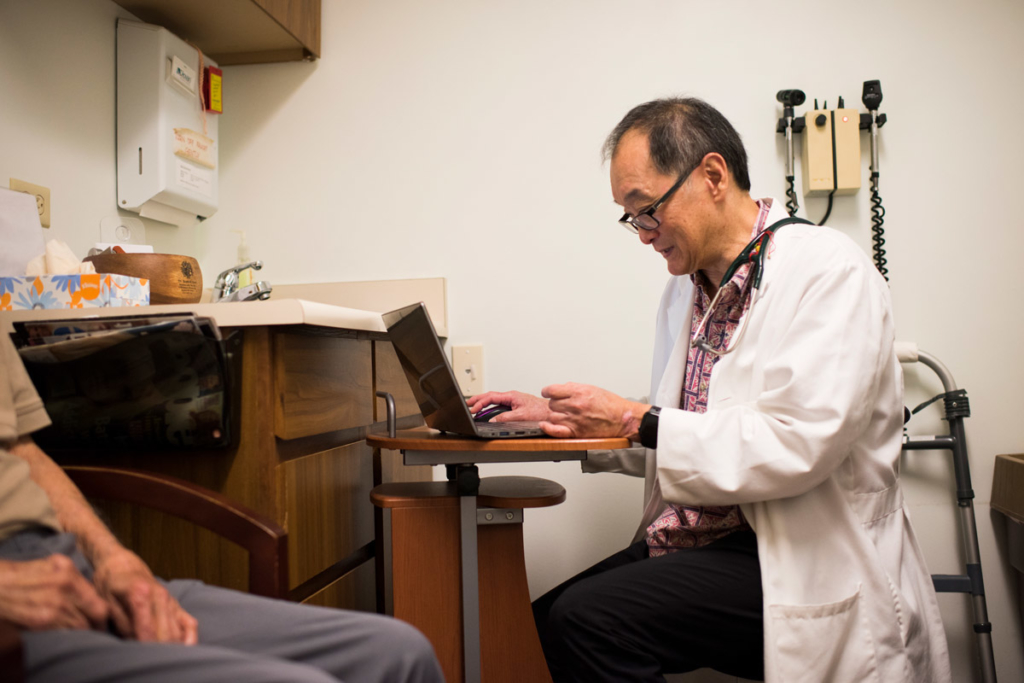
- Focus on quality improvement. Dr. Kimura prioritizes evidence and evolution, which means he must also prioritize data collection and analysis. By leveraging his EHR system and employee input, Dr. Kimura evaluates processes, adjusts protocols, and capitalizes on opportunities for improvement. “If anybody practices in a way where there’s never any change, they’re going to be left behind,” he says.
- Adopt an EHR system with a human-centered design. For six years, Dr. Kimura used an EHR that caused more headaches than happiness. After learning of Elation Health from receiving a referral letter from another doctor, he became the second doctor in Hawai‘i to adopt the technology. The system’s focus on efficiency meant Dr. Kimura could keep his patients at the forefront. He points to his EHR as a defense against burnout, a rare sentiment among physicians.
- Participate in innovative value-based payment programs. Dr. Kimura joined a program payment transformation initiative through the Hawaii Medical Service Association, an insurer affiliated with Blue Cross Blue Shield. The program provides monthly capitation payments for each member who identifies as a patient of Dr. Kimura, regardless of how often they come in for an appointment. To maintain payment levels, Dr. Kimura must document his adherence to quality care and appropriate patient access and hit certain goals. Overall, he says, the value-based care effort has increased time spent with patients and provided a steady stream of revenue.
Hawai‘i’s healthcare system faces an uncertain future, distinct from the uncertain future of the mainland’s system. The state is already battling an especially severe physician shortage, thanks in part to subspecialties that require medical residents to leave for the continental United States. Once there, they often don’t come back.
“A lot of us in Hawai‘i feel an obligation to our patients and to our community,” Dr. Kimura says, “so we practice to an older age than primary care docs probably do on the mainland.”
There’s little doubt that Dr. Kimura, nearing his fourth decade in medicine, feels compelled to continue. To keep those Saturday appointment hours. To make house calls. To spend those few extra, sometimes critical, minutes listening to each patient. Just like he always has.