MACRA Monday: Resource Use
MACRA Monday: Resource Use December 12, 2016
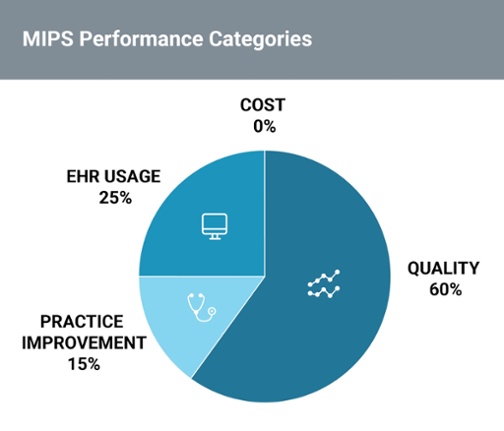
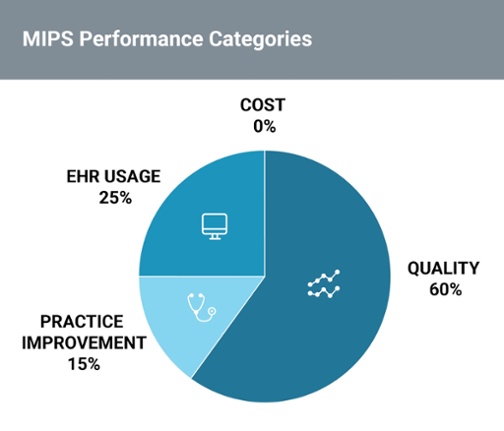
Join us on Mondays for our MACRA Monday series to hear how we break down the four performance categories that independent practices will be required to report on when MACRA and MIPS goes into effect on January 1.
The fourth and final performance category for MACRA is the “Resource Use” or “Cost” performance category which replaces the Value Modifier (VM) Program. VM currently provides an adjustment based on the quality and cost of care provided to people with Medicare under the Medicare Physician Fee Schedule.
Though Resource Use will not contribute to the overall MIPS score during the first year, starting in 2018, Cost will account for 10% of your score and 30% during the subsequent year.
What are the requirements?
This new category predominantly measures quality through cost. Unlike other MIPS categories, providers do not need to report anything to CMS in order to attest for this performance category. Instead, CMS gathers the data from your practice’s Medicare claims to make adjustments.
Comparing Resource Use with the Value-Based Payment Modifier
Overall, the Resource Use performance category is similar to VM but aims to simplify aspects of the program. One key difference is that the Resource Use performance category adds 40+ episode specific measures to address specialty concerns.
| Value Modifier | Resource Use |
| 6 measures:
Total per capita costs for all attributed beneficiaries, Medicare Spending per Beneficiary (MSPB), Total per capita cost measures for the four condition-specific groups (chronic obstructive pulmonary disease, congestive heart failure, coronary artery disease, and diabetes mellitus). Attribution to the group practice (TIN) |
2 of the 6 VM measures: Total per capita costs for all attributed beneficiaries, Medicare Spending per Beneficiary (MSPB), Removes total per capita cost measures for the four condition-specific groups. Proposes up to 41 other episode based measures. Attribution to group (TIN) or individual (TIN/NPI) |
How is Resource Use calculated?
The score for the Resource Use performance category score is calculated by CMS by taking the information from a provider’s claims and converting each measure into points. These points are then divided by the total possible points available to a provider to come up with a final score for this category. A primary care provider in a solo practice, like the example provided below, might calculate their score like this:
| Dr. Joy Smith’s claim data: |
|
Type of Measure |
Number of Cases |
Performance |
Measure Performance Threshold |
Points Based on Decile |
Total Possible Points |
|
| MSPB | 20 | 15,000 | 13,000 | 4.0 | 10 | |
| Total Per Capita | 21 | 12,000 | 10,000 | 4.2 | 10 | |
| Episode 1 | 22 | 15,000 | 18,000 | 5.8 | 10 | |
| Episode 2 | 10 | 11,000 | 9,000 | Below Case Threshold | N/A | |
| Episode 3 | 0 | N/A | N/A | No Attributed Cases | N/A | |
| Episode 4 | 45 | 7,000 | 10,000 | 8.3 | 10 | |
| Total | 22.3 | 40 |
Key Takeaways:
- The Resource Use performance category aims to measure quality of care through cost.
- Resource Use will account for 0% of your score in 2017, but starting in 2018, “Cost” will account for 10% of your score and 30% the following year.
- This performance category has no reporting requirements; CMS gathers the data from Medicare claims meaning your reporting burden is reduced.
Subscribe to our MACRA Resource Series to recieve content like this straight to your inbox!
Related Posts:
- Everything you need to know about MACRA and its final rule
- Quality Performance Category
- Advancing Care Information Performance Category
- Clinical Practice Improvement Performance Category
![]()







