What Does MACRA Mean? What You Need to Know Now (Plus Its Final Rule)

After months of waiting, CMS released the final piece of guidance for the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), also known as the Quality Payment Program. With this final rule, Centers for Medicare Medicaid Services (CMS) took the golden opportunity to listen to hoards of physician feedback on the potential impact of this new reimbursement program on small independent practices.
The result?
CMS, through this most recent revision to the rule, has now significantly lessened the burden of transitioning and attesting to these new requirements for small and independent practices, as we detailed in an earlier post.
Though we’re quickly approaching MACRA’s January 1, 2017 start date, 50 percent of physicians say they’ve never even heard of the law and 32 percent of the doctors that recognize MACRA’s name are unfamiliar with its requirements.
We’re here to help. With all of the demands on a clinician’s time, sifting through dense policy requirements should be last on a to-do list. So read on below, and we’ll spell out key takeaways about MACRA and what you can anticipate come January 1.
Background on MACRA
First, let’s start off with how we got here. MACRA streamlines current fee-for-service Medicare programs (Meaningful Use, Physician Quality Reporting System, and Value-Based Payment Modifier) into a single program. There are two tracks for physicians, the Merit-based Incentive Payment System (MIPS) or participating in an Alternative Payment Model (APM). MACRA repeals Medicare’s old methodology for determining reimbursement amounts, the unpopular and flawed sustainable growth rate (SGR) methodology or “the doc fix”, that Congress would annually repeal to avoid extreme pay cuts for physicians.
MACRA will go into effect in 2017. This means that in 2017, CMS will start collecting reporting from providers in order to set benchmarks for their performance in the key domains that MIPS will measure. The first year that MACRA affects physician pay will be 2019.The four performance categories used for scoring are:
• Quality of care
• Cost of care
• Practice improvement measures
• EHR usage
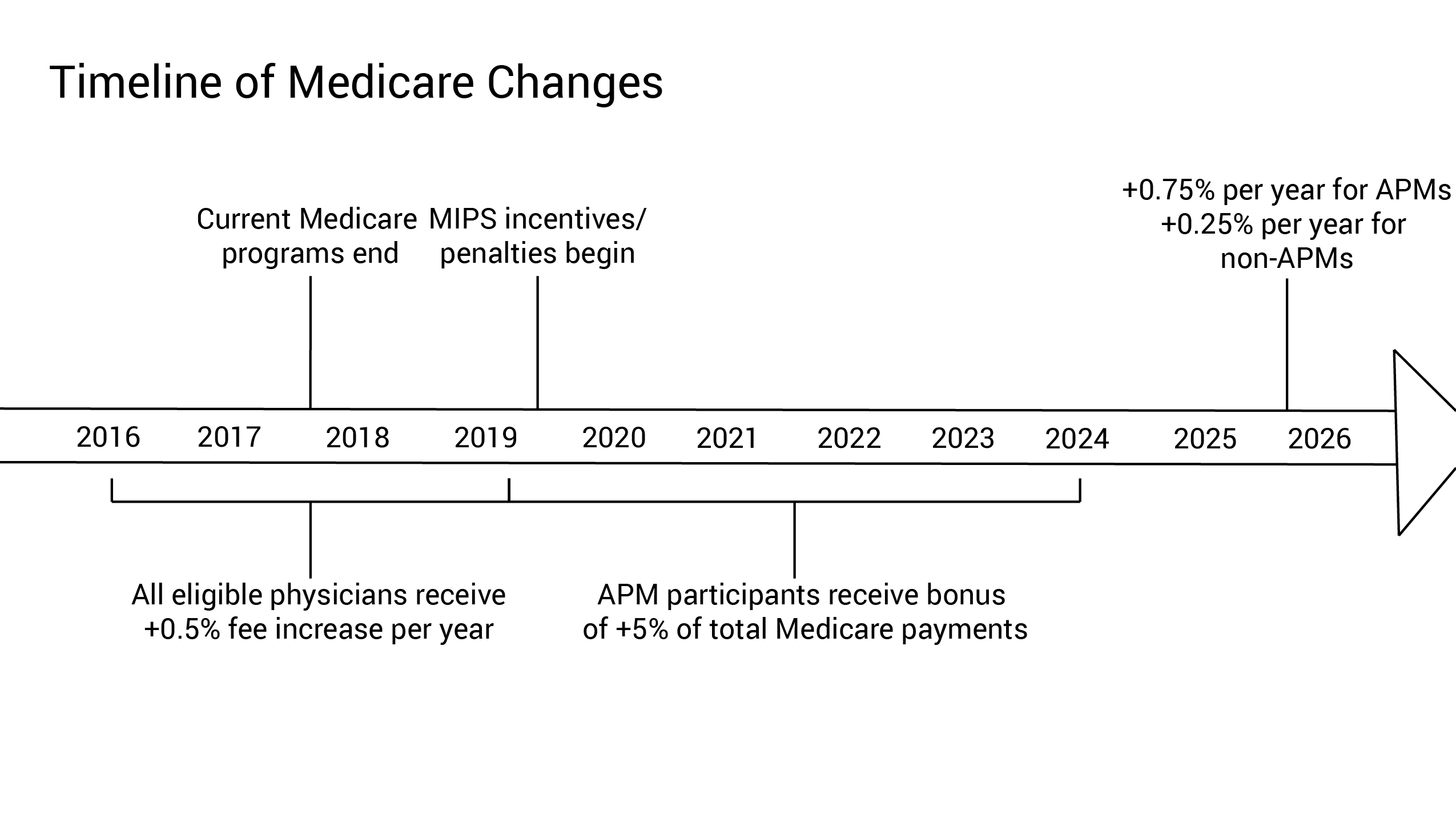
The second rule, which came out in September, eased the path toward MACRA by establishing four different tracks for when clinicians need to participate in the program. No matter what track providers choose, participants will not be penalized during the first year of MACRA.
The Final Rule
So what changed from the initial draft of MACRA to the final one, released last week? In a nutshell, CMS made room for many more exemptions from the program and introduced more flexibility for physicians to make choices about how to participate. We’ll summarize below:
• More flexible timing. ;CMS has implemented transitional scoring and reporting policies for this first year. Due to the phased approach, more than 90 percent of MIPS eligible clinicians should receive a positive or neutral payment adjustment, and at least 80 percent of clinicians in small and solo practices should receive a positive or neutral payment adjustment, in 2019 which is the first year of adjusted payments under the new law.
• Lower minimum requirements for providers. CMS increased the Medicare low-volume threshold which exempts more providers from either model. Specifically, the low-volume MIPS exclusion threshold is now $30,000 of Medicare billings or fewer than 100 Part-B beneficiaries, which will greatly increase the number of small practices that are exempt from MIPS.
• Creation of new exemption tracks. More clinicians can qualify for be exempt from MIPS through participating in an Alternative Payment Model (APM). CMS will create a new MSSP Track 1+ model to qualify clinicians for Advanced APM treatment, and reopen several current models to enable more physicians to become Qualifying Alternative Payment Model Participants (“QPs”).
• More financial flexibility. CMS has eased requirements to qualify as an APM. Also, the definition of participating in a patient-centered medical home (“PCMH”) has expanded, which increases the possibilities of favorable scoring for practices in the Improvement Activities domain of MIPS.
• Reduced reporting burdens. In the first performance year, the Cost/Resource Use performance domain has been eliminated for all physicians and clinicians. Requirements for reporting in the Advancing Care Information domain decreased from eleven necessary measures, to five. Opportunities for bonus points in the Improvement Activities domain, including participating with certain EHR technology activities, has increased.
• New standards for high and low performance.In 2017, CMS set a Performance Threshold of 3, which will result in a physician/clinician scoring less than 3 receiving a negative payment adjustment (-4 percent). A score of 3 can be achieved by submitting, for example, just a single Quality Measure in reporting. Clinicians who choose not to submit a report on a single measure or activity will receive the full negative adjustment of 4 percent. Also in 2017, CMS set an Exceptional Performance Threshold at 70, resulting in a physician/clinician scoring above 70 becoming eligible for additional funds from the $500 million exceptional performance pool.
How will this affect my practice?
The changes to MACRA in the final rule should reduce the initial impact on small practices. CMS revised its QPP participation estimates, projecting that about 70,000 to 120,000 clinicians will become QPs in 2017—an increase from the 30,000 to 90,000 estimate in the Proposed Rule—and about 125,000 to 250,000 will become QPs in 2018. CMS estimates that approximately 592,000 to 642,000 eligible clinicians will be required to participate in MIPS in 2017.
Physicians will also have more time to learn and adjust to the new policy. Because of the challenges faced by providers in adopting MIPS for CY 2017, a number of temporary transitional provisions have been enacted. Providers can pick their pace of participation, with even the smallest submission preventing negative adjustment.
So what’s next?
All clinicians must prepare to report on care quality in 2016.Quality will make up 60% of MIPS measurement in the first year, and clinicians who report just a single quality measure in 2017 can avoid a negative reimbursement. It is essential that providers are prepared for this reporting, and EHR vendors need to be ready to assist.
We’re Here to Help
Policy changes can feel daunting and frustrating at any level, particularly for a small or solo practice. Our number one concern has always been to ensure independent physicians feel empowered — not overwhelmed — to deliver the high quality care they are known for.
We’ve sifted through policy, stayed on top of the changes, and done our homework — so that you don’t have to. With our resource series,you can have access to our live webinars, informative videos, email newsletters, detailed articles, and health policy specialists on-call to give you specific guidance and support. And with our clinical first EHR, you can always be sure that you have an EHR system equipped with the robust quality care measures and intuitive reporting tools that can help you strengthen the physician-patient relationship and enable phenomenal care for all.







